The Hidden Truths about Weed
For those who may not know me, I’m Dr. Julie Berry. I graduated with my doctorate in pharmacy many years ago and have had the honor to work in a variety of healthcare settings. Early on in my education, I developed a passion for those struggling with various forms of addiction and in my last didactic year, did my doctoral presentation on the negative effects of hookah, a topic that was both prominent yet wildly misunderstood while I was in school. The long story short was that hookah, despite its form (water based versus not), is incredibly dangerous in increasing one’s risk of lung cancer, COPD, and cardiovascular disease.
In later years, cannabis use has become the hot and trendy topic. I’ve been approached numerous times about signing petitions for the legalization of marijuana. I’ve known people who use. I’ve been slapped with the aroma of it while driving on I-95.
My aim is not to discuss policy. One of my greatest responsibilities as a pharmacist is to educate. One of the most well known public service announcements has been the DARE campaign, the Tobacco Free Florida campaign… so many people in the 50s and 60s were addicted to smoking and had no idea the impact it was having on their health.
In this day and age, with the access we have to information, we have no excuse to be ill-informed. I want you to know the very real risks of marijuana use so that you can make an informed decision for yourself.
Marijuana use dampens the brain’s natural response to reward
Image credit: PsyPost.
A recent clinical trial conducted brain scans of marijuana users and non-users after receiving a monetary reward. What they found was that marijuana users had a lower response to receiving a monetary reward compared to non-users. Dr. Heitzeg, senior author and U-M neuroscientist of this study said it this way: "This means that something that would be rewarding to most people was no longer rewarding to them, suggesting but not proving that their reward system has been 'hijacked' by the drug, and that they need the drug to feel reward — or that their emotional response has been dampened." (9)
Using functional magnetic resonance imaging (fMRI), they found that marijuana use is associated with a diminished response in the nucleus accumbens (NAc), a structure that plays a major role in the brain’s reward system. (8) The nucleus accumbens is heavily involved in the release of dopamine in response to rewarding stimuli (such as food, sex, or addictive substances), playing a key role in motivation, behavior, and pleasure. Since it has various functions, it is involved in many neurological and psychological disorders including addiction, OCD, anxiety, depression, Alzheimer’s, Parkinson’s, and obesity. (10)
Dr. Heitzeg goes on to say, “Some people may believe that marijuana is not addictive, or that it's 'better' than other drugs that can cause dependence. But this study provides evidence that it's affecting the brain in a way that may make it more difficult to stop using it.” (9)
It can be addictive
According to the National Institute on Drug Abuse, “marijuana use can lead to the development of problem use, known as a marijuana use disorder, which takes the form of addiction in severe cases. Recent data suggests that 30 percent of those who use marijuana may have some degree of marijuana use disorder.”
Those with marijuana use disorders often develop dependence on marijuana and can experience withdrawal symptoms such as “irritability, mood and sleep difficulties, decreased appetite, cravings, restlessness, and/or various forms of physical discomfort,” when trying to quit. (12)
Reduced cognitive function
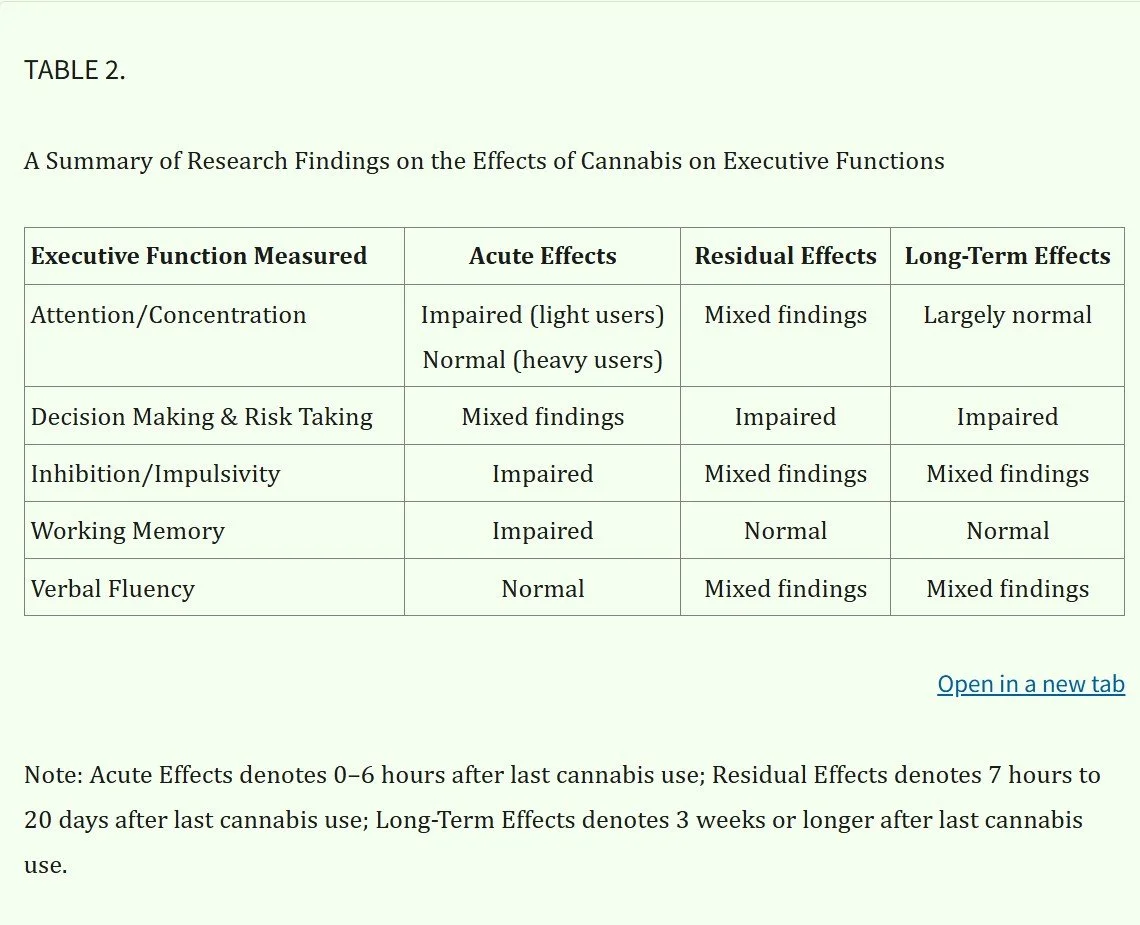
An evidenced-based review published by the Journal of Addiction Medicine showed that cannabis use can affect a variety of cognitive functions in the short-term as well as long-term. “Cannabis use has been shown to impair cognitive functions on a number of levels—from basic motor coordination to more complex executive function tasks, such as the ability to plan, organize, solve problems, make decisions, remember, and control emotions and behavior.” (11)
Although long-term effects of cannabis on cognitive function are most apparent with chronic, heavy users, “even occasional cannabis use can acutely impair attention, concentration, decision-making, inhibition, impulsivity and working memory.” The table below summarizes their findings.
Marijuana Induced Psychosis
Image credit: Drug Free America Foundation, Inc.
This is arguably one of the biggest risks of marijuana use that seems to be largely ignored in the media. Despite this, there are many studies that address this phenomenon.
A recent study published by the American Journal of Psychiatry illustrated the connection between marijuana use and various psychotic disorders. Nearly 80,000 Americans were surveyed from 2001–2002 and 2012–2013 and found that cannabis use was significantly associated with self-reported psychotic disorders. (13)
Another publication by World Psychiatry took a look at multiple longitudinal studies to examine the relationship between cannabis use and the risk of psychosis. After adjusting for various confounding variables such as other forms of drug use and other personal characteristics that predict an increased risk of psychosis, they found that, “there is now reasonable evidence… that regular cannabis use predicts an increased risk of schizophrenia and of reporting psychotic symptoms.” (2) This relationship is likely due to cannabis interacting with the dopamine neurotransmitter system which is involved in psychotic disorders.
A study conducted by the London Health Sciences Centre Canada also confirmed this troubling connection. Check out their brief overview of the study in the video below:
Increased risk of depression
Now I know what you may be thinking… don’t people use marijuana to help with their depression? This is what the American Psychiatry Association says…
“There is no current scientific evidence that cannabis is in any way beneficial for the treatment
of any psychiatric disorder. In contrast, current evidence supports, at minimum, a strong
association of cannabis use with the onset of psychiatric disorders. Adolescents are particularly
vulnerable to harm, given the effects of cannabis on neurological development. ”
There are many studies to support this consensus statement. Cannabis use may lead to the onset of depression and worsen the prognosis in those already diagnosed with Major Depressive Disorder. (16,17)
An Australian cohort study analyzed 1600 teenage students over the course of 7 years and found staggering statistics between cannabis use and the incidence of anxiety and depression. After adjusting for confounding variables such as other drug use, they found that daily use of cannabis in young women was associated with a five times greater likelihood of also reporting anxiety and depression. Teens using cannabis once weekly or more resulted in about a two times greater risk for developing later anxiety and depression. (3)
A large cohort study from Denmark that analyzed over 6 million patients found that “cannabis used disorder was associated with an increased risk of both psychotic and nonpsychotic unipolar depression and bipolar disorder.” (14)
The Bottom Line
Marijuana can reduce the brain’s natural response to reward, can be addictive, cause cognitive dysfunction and/or psychosis, and can increase your risk of developing a psychiatric disorder (or worsen it if you already have it).
As someone who works in healthcare and has seen many loved ones struggle with various psychiatric illnesses, I can tell you that I am someone who can empathize with those who are struggling mentally. From my years of study and research, I’d like to encourage you…
There are lots of options out there for those who may be struggling.
Since I am a pharmacist, I would like to put it out there: If you are someone who takes a medication for your mental health and you’re not happy with it (if it’s not effective for you, if you’re experiencing some unwanted side effects, etc.), please don’t hesitate to let your provider know! There are many medication options out there (SSRIs, SNRIs, DNRIs, TCAs, atypical antipsychotics, SPARI, SMS, etc), so don’t feel like you’re stuck if one isn’t working for you.
From making lifestyle adjustments in diet and exercise to seeing a therapist/psychologist to various FDA approved medications to getting plugged into an uplifting community to prioritizing your spiritual well-being (reading the Bible, praying, going to church), a wholistic approach can be really helpful in your mental well-being. Please never struggle alone. If you’re feeling down, tell a loved one (or multiple!) and let them come alongside you.
References:
1) Arendt M, Rosenberg R, Foldager L, Perto G, Munk-Jørgensen P. Cannabis-induced psychosis and subsequent schizophrenia-spectrum disorders: follow-up study of 535 incident cases. Br J Psychiatry. 2005 Dec;187:510-5. doi: 10.1192/bjp.187.6.510. PMID: 16319402.
2) Hall W, Degenhardt L. Cannabis use and the risk of developing a psychotic disorder. World Psychiatry. 2008;7(2):68-71. doi: 10.1002/j.2051-5545.2008.tb00158.x. PMID: 18560513; PMCID: PMC2424288.
3) Patton GC, Coffey C, Carlin JB, Degenhardt L, Lynskey M, Hall W. Cannabis use and mental health in young people: cohort study. BMJ. 2002 Nov 23;325(7374):1195-8. doi: 10.1136/bmj.325.7374.1195. PMID: 12446533; PMCID: PMC135489.
4) Hall W, Degenhardt L. What are the policy implications of the evidence on cannabis and psychosis? Can J Psychiatry. 2006 Aug;51(9):566-74. doi: 10.1177/070674370605100904. PMID: 17007223.
5) https://www.lhscri.ca/news/new-study-reveals-potential-biological-link-between-cannabis-use-and-psychosis/
6) https://medicine.yale.edu/news-article/behind-the-smoke-unmasking-the-link-between-cannabis-and-schizophrenia/
7) Levi L, Bar-Haim M, Winter-van Rossum I, Davidson M, Leucht S, Fleischhacker WW, Park J, Davis JM, Kahn RS, Weiser M. Cannabis Use and Symptomatic Relapse in First Episode Schizophrenia: Trigger or Consequence? Data From the OPTIMISE Study. Schizophr Bull. 2023 Jul 4;49(4):903-913. doi: 10.1093/schbul/sbad033. PMID: 36999551; PMCID: PMC10318873.
8) Martz ME, Trucco EM, Cope LM, et al. Association of Marijuana Use With Blunted Nucleus Accumbens Response to Reward Anticipation. JAMA Psychiatry. 2016;73(8):838–844. doi:10.1001/jamapsychiatry.2016.1161
9) https://www.michiganmedicine.org/health-lab/over-time-marijuana-use-dampens-brains-response-reward
10) Harris HN, Peng YB. Evidence and explanation for the involvement of the nucleus accumbens in pain processing. Neural Regen Res. 2020 Apr;15(4):597-605. doi: 10.4103/1673-5374.266909. PMID: 31638081; PMCID: PMC6975138.
11) Crean RD, Crane NA, Mason BJ. An evidence based review of acute and long-term effects of cannabis use on executive cognitive functions. J Addict Med. 2011 Mar;5(1):1-8. doi: 10.1097/ADM.0b013e31820c23fa. PMID: 21321675; PMCID: PMC3037578.
12) https://flboardofmedicine.gov/forms/is-marijuana-addictive.pdf#:~:text=Marijuana%20use%20can%20lead%20to%20the%20development,the%20form%20of%20addiction%20in%20severe%20cases.&text=Those%20studies%20suggest%20that%209%20percent%20of,those%20who%20start%20using%20in%20their%20teens.
13) Livne O, Shmulewitz D, Sarvet AL, Wall MM, Hasin DS. Association of Cannabis Use-Related Predictor Variables and Self-Reported Psychotic Disorders: U.S. Adults, 2001-2002 and 2012-2013. Am J Psychiatry. 2022 Jan;179(1):36-45. doi: 10.1176/appi.ajp.2021.21010073. Epub 2021 Oct 14. PMID: 34645275; PMCID: PMC8945254.
14) Jefsen OH, Erlangsen A, Nordentoft M, Hjorthøj C. Cannabis Use Disorder and Subsequent Risk of Psychotic and Nonpsychotic Unipolar Depression and Bipolar Disorder. JAMA Psychiatry. 2023;80(8):803–810. doi:10.1001/jamapsychiatry.2023.1256
15) https://www.psychiatry.org/getattachment/12aa44f8-016e-4f8c-8b92-d3fb11a7155f/Position-Cannabis-as-Medicine.pdf
16) Feingold D, Weinstein A. Cannabis and Depression. Adv Exp Med Biol. 2021;1264:67-80. doi: 10.1007/978-3-030-57369-0_5. PMID: 33332004.
17) Sorkhou M, Dent E, George T. Front Public Health. 2024 Apr;12. https://doi.org/10.3389/fpubh.2024.1346207